The Challenge of CAR-T Therapy: From Genetic Therapy to Brain Vaccines and Artificial Cellular Receptors in the 21st Century
Researchers around the world can have the same talks with their regulators, even in a normal hot spot for drug development such as the United States and Europe. Such conversations will help to prepare for a future in which bespoke genetic therapies can be produced worldwide. Helping to harmonize regulations between countries is an important goal for promoting the development of drugs for conditions that affect only a few individuals scattered around the globe.
Today, the chatter is very different. Engineered CAR T immune cells have so far been used to treat more than 30,000 people with cancer in the United States alone. CAR-T therapy is being tested for other conditions, including some severe autoimmune disorders. The commercial success of CAR T cells was US$8.3 billion in 2023.
Both approaches are fraught with challenges. As in the early days of CAR-T therapy, many of them are not scientific. But by guiding regulators and developing flexible platforms for producing bespoke treatments, researchers can help to shepherd therapies to the people who need them.
Researchers have long chased after vaccines that could rally the immune system against tumours, similarly to how vaccines rouse defences against pathogens. Companies can now sequence portions of a person’s tumour and select those most likely to be visible to the immune system. The synthesis and encapsulated production of the mRNA molecules correspond to those regions and are similar to the production of the COVID-19 vaccines. It takes as little as a month to complete the process.
Even though it is rare, people with a genetic condition can be beneficiaries of these technologies. But the reality is harsher. It will take a long time to put together the techniques needed for rapid, on-demand, custom CRISPR therapies. Most people with these conditions don’t have that kind of time.
Ghosh and his collaborators were racing to design a one-off treatment that would edit the DNA in the 20-year-old woman’s brain cells and get them to stop producing toxic proteins. It was an approach that had never been tried before, with a long list of reasons for why it might not work.
The team seemed to be on its way to the finish line. Many of the researchers were working 10-to-12-hour days, and it was nearly time to test their therapy in mice. He needed the approvals by the time the animal results were in, so he was scheduling a regulatory inspection. The surgeon would perform Uditi’s injection.
The family of Uditi wanted to do this project because they believed that the work they did on this project could help future attempts to develop therapies for genetic conditions.
Uditi was always in a hurry as a young girl. She would make sure to get her mother ready for a festival hours in advance, because she wanted to celebrate regardless of what it was. She greeted family and friends with cuddles and kisses and brightened parties with her laughter and dancing.
For the first nine years, there was no hint of trouble. It was just a brief flicker when Uditi would start to move.
She’d switch back on again as if nothing had happened, and her mother, Sonam, wasn’t sure if she should worry. But then Sonam saw nine-year-old Uditi drop a camera on the floor and become confused as to why it was no longer in her hand. A mother’s hunch hardened: something was wrong.
The doctors told her that she had ecsymy. When Uditi’s seizures became more pronounced and she began to struggle at school, Sonam and Rajeev, Uditi’s father, decided it must be something more. They took part of Uditi’s genome last year.
While studying online, the Sarafs discovered Indian ayurvedic treatments, a ketogenic diet, special schools, seeing a lot of physicians and trying out various medicines. “We shopped for doctors. We shopped for gods,” says Sonam, but Uditi’s condition slowly worsened.
Even if each of these hurdles were surmounted, at best, base editing might stop the production of neuroserpin clumps in some of Uditi’s neurons. The treatment was unlikely to reach all affected cells, and it was unlikely to clear the clumps that were already present or to regenerate neurons that had been lost.
This condition is called FENIB (familial encephalopathy with neuroserpin inclusion bodies), and the symptoms — which can be similar to dementia — usually manifest late in life. Elena Miranda, a cell biologist at the Sapienza University of Rome, runs the world’s only lab that focuses on the disease. She says that it’s possible that many cases of FENIB go unreported because physicians do not often sequence the genomes of older adults with dementia.
Uditi and her family journeyed on a lonely journey. They had never heard of FENIB, and neither had Uditi’s physicians. Sonam did some research but couldn’t bring herself to fully absorb what she found. She says they didn’t think it was possible. It can’t happen with our daughter.
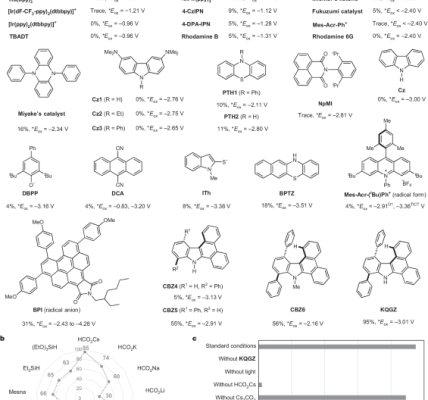
Uditi’s disease was caused by a mutation that converts a single DNA base from a ‘G’ to an ‘A’. A variation on CRISPR genome editing, called base editing, could theoretically correct exactly this kind of mutation (see ‘Precision gene repair’).
Devinsky also emphasized the difficulties. Base editing had never been tested in a clinical trial at that time. The technique involves taking a large proteins and a small piece ofRNA and putting them in affected cells. The brain is one of the most daunting organs and researchers are trying to perfect this delivery.
Preliminary studies of the approach were to be conducted by a team of NYU Langone Health experts. The researchers pulled together what funding they could from other grants, and the Sarafs funded the rest. Sonam said they will sell their house if they have to.
The pressure in the lab was intense, says team member Jayeeta Basu, a neuroscientist at NYU Langone Health. The team genetically engineered Uditi’s FENIB mutation into cells grown in the lab. When the cells initially did not seem to perform as they were supposed to, the graduate student was asked multiple times to repeat the experiment. She says she was always pushing. “We had to be fast, but we also had to be diligent. There was no short cut.”
AAV-Based Therapy for Sickle-cell Disease in India: a Memorino from a Conversation with Uditi Sarafs
In December 2019, the Sarafs moved back to India. Maintaining a home in the United States was expensive, and Uditi missed her extended family. In January of 2021, Uditi was hospitalized after getting hit by the COVID-19 Pandemic. Sonam says that her health was never the same after she spent 20 days in the hospital. Uditi couldn’t communicate with anyone and she had to pace the house constantly, so she never went to sleep.
A US foundation had been petitioned to come up with antisense therapy for Uditi. Her family flew from India to the United States for the injections. She could not understand the world around her on the trips.
Rajeev and Sonam went to the institute to talk to Chakraborty and the institute’s director, chemist Souvik Maiti, who had been collaborating with Chakraborty on the CRISPR technology behind the sickle-cell project.
Most of the people with sickle-cell disease in India — a country with one of the highest rates of the condition — live in impoverished communities. Chakraborty and his colleagues hoped to develop a therapy that could be produced and administered at a fraction of the price that is charged in the United States, if not less.
With funding, Maiti and Chakraborty took some time to discuss the project with the person who was building a facility in Bengaluru to produce viruses that are often used in gene therapies. Ghosh aimed for his facility to be one of the first in India to produce AAVs to the standards required for use in people.
It wasn’t the first time that Ghosh was swayed by a personal appeal: in the years before he met Uditi he found two women waiting outside of his office. The women said that they wouldn’t leave until he came up with a cure for their young sons’ illness, which can be fatal if left undetected. The women pledged to help raise funds, and Ghosh found himself unable to say no. Since then he has become close to the families and worked on the project.
India has earned a reputation for making complex drugs on a budget. During the COVID-19 pandemic, Indian manufacturers cranked out millions of doses of vaccines. The country is making a Malaria vaccine at a fraction of the price in Europe and it is also developing cell andgene therapies that cost less than those in the United States.
Source: Hope, despair and CRISPR — the race to save one woman’s life
Using AAVs to Identify the Strains that Should be Injected into Uditi’s Brain Neurons
The lead on Uditi’s project was taken by Chakraborty. Rya Rauthan, who was a PhD student in the lab, says that he is a go-getter kind of person. “He is not bothered by who he needs to ask to get something done, he just does it.”
To minimize interruptions, the team mapped out all of the experiments and the components they would need from start to finish. Many lab reagents have to be imported and supply disruptions can delay projects for weeks or months. Everything had to be planned and ordered ahead of time, and Maiti worked to keep the supplies coming, seeking out vendors and negotiating prices. “Time was more valuable than anything else,” he says.
Stem cells were derived from samples of Uditi’s blood. Then, she and her colleagues coaxed those cells to become neurons, and used base editing on them in the lab.
The AAV that was prepared was to be used to bring the components to Uditi’s neurons. The team needed to figure out which strain would work best in order to protect the brain. Ghosh’s lab tested several types of AAV in mice, to find out which one caused the least amount of inflammation and how best to administer it. The team eventually settled on one type — called AAV9 — and determined that it should be injected directly into Uditi’s brain.
Others in the lab also took the news hard. For clinicians, it could be that they become hardened. “We don’t have that experience. We were hurting.