An Experimental Investigation of Parkinson’s Disease in a Walnut-Shaped Deep-Brain Structure Using Thawed, Transplanted Neurons
Just before surgery, the cells were thawed and injected into a walnut-shaped, deep-brain structure called the putamen, which is an important motor-relay station. People with Parkinson’s disease have a weakness that extends out to the putamen.
The results published in March show that the cells are unharmed one year after surgery for three individuals. There are some signs of benefit. One of the three individuals said she could see her husband’s face clearly for the first time in ten years, but only through a small section of her eye, where the cells had been transplanted.
The trials were mainly designed to test safety, which isn’t enough to say if the intervention is effective.
Some people got better and others didn’t get worse, that could be because the number of cells they transplant is small in the first few trials.
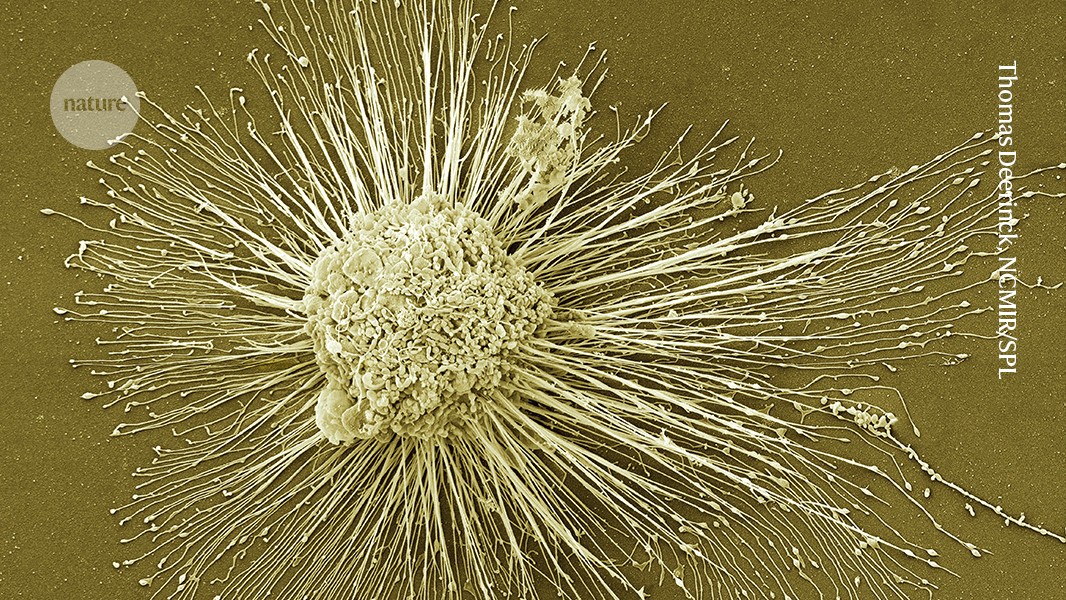
Parkinson’s is a neurological condition caused by loss of dopamine- producing neurons that cause tremors, stiffness and slowness in movement. There is currently no cure for the condition, which is projected to affect 25 million people globally by 2050.
The effects of stem cell transplantation on MDS-UPDRS part III: a Japanese case study and its implications on motor symptoms in adults and young children
The stem cells were injected in 18 different places across the putamen to fill up the brain area that was missing.
Five individuals received a dose of 0.9 million cells and 7 received 2.7 million cells, in the hope that 100,000 and 300,000 cells, respectively, would survive the surgery. A healthy brain typically has 300,000 dopamine-producing neurons. The recipients were given immune-suppressing drugs for one year after the surgery to prevent their bodies from rejecting the transplant.
Brain scans showed an overall increase in dopamine production, suggesting that some neurons survived the entire 18-month observation period, even after the participants stopped receiving immune-suppressing drugs.
The individuals who received the lowest dose showed a 9 point improvement in their symptoms compared to the individuals who received the highest dose. The assessment measures things like eating and sleep. Stem-cell scientist Agnete Kirkeby, who is working on a European trial, believes that the results need to be larger because this metric can be swayed by the placebo effect.
The second study2, conducted in Japan, started with adult cells from a donor and reverted them to a pluripotent state, from which they could be coaxed into becoming neural progenitor cells. Freshly differentiated cells were immediately injected into participants, comprising four men and three women aged 50–69.
300,000 and 150,000 cells, respectively, were expected to survive after four people received up to 11 million cells. Jun Takahashi is a neurosurgeon at Kyoto University in Japan and he leads the trial that looked at low survival rate. The participants were given immune-suppressing drugs.
The benefits of the three patients who showed a beneficial effect on MDS-UPDRS part III are shown by their off-time period and scores. The patient’s perceptions are reflected in these evaluations. It is possible that patients had very high expectations for this new treatment, and the results did not meet such high expectations despite objective improvements. In the remaining two patients (PD05 and PD06), motor deficits stabilized at a similar level of decline to those receiving conventional medication36,37. The two patients had worse motor symptoms while on the clock, suggesting that the beneficial effects of the grafts were diminished by slower neurodegeneration in the non-dopaminergic systems. PD05 was 69 years old at the start of the study, and younger patients with less severe symptoms appear to be more suitable for this treatment. Considering these results, refining patient eligibility criteria may enhance the efficacy of this treatment.
There were discrepancy between the Hoehn–Yahr stage scores and the MDS-UPDRS part III scores. Punctual instability and mobility issues are emphasized by the Hoehn–Yahr stage, whereas the MDS-UPDRS part III has a more comprehensive evaluation of major motor symptoms in the disease. The improvement in the Hoehn–Yahr stage has been linked to improved stability and mobility as compared to the changes seen in the other parts of the study.
The Path to Regenerative Medicine in Japan: A Case Study of Masayo Takahashi, the First Person to Transplant Cells from iPS Cells
Scientists started clinical trials. Big companies invested more in manufacturing hubs. A large number of patients from Japan and abroad will be coming to the medical facilities. “Regenerative medicine in Japan is moving very dramatically,” says Masayo Takahashi, an ophthalmologist at Kobe City Eye Hospital and president of the biotechnology company, Vision Care. She was the first person to treat someone with cells from iPS cells.
Many countries are exploring how to get drugs and therapies to market more quickly. Japan is currently in the spotlight, with a slew of its universities, companies and funding bodies preparing to apply for fast-tracked regulatory approval for certain products based on iPS cells, in some cases perhaps even within the year, as we report in a News Feature.
But those approvals are not yet in hand, treatment costs are high, large trials showing clear clinical benefit have yet to materialize, and concerns about safety could still sap the public’s willingness to try this treatment. “We’re down to realizing what the potential of these cells are, and what the limits are,” Shimmura says.
Yamanaka’s iPS cells promised to bypass a bioethical stand-off that had threatened the potential of embryonic stem cells for a decade. iPS cells are not required to destroy human embryo in order to be ethically less fraught. Furthermore, because they could be made from the cells of the person in need of treatment, they promised to offer transplantable tissues without the need for immune-suppressing drugs.
They tried injecting donor cells just under the retina but didn’t work out. But the researchers had limited control over where the cells grew. Next up, they tried growing strips of cells, 2 centimetres long and 200 micrometres thick. They used a tube to slide several of these strips onto the retina through a tiny incision in the eye, in the hope that they would expand into sheets.
It was a procedure with limitations. Cell therapies are timeConsuming and Costy, as well as the large cell sheets that were designed for implantation required intrusive surgery. To demonstrate to the world what was possible, it was her choice to use this approach. It was meant to be the best treatment.
The difficulties might come down to the retina’s natural resistance to regeneration. The clear covering that lets light in, the cornea, could use more cell therapies, as it is maintained by a pool of stem cells and constantly being rebuilt.
The future of iPS cells: how fast should innovation be allowed? A Japanese expert on the biomedical aspect of the fast-track process
Nishida has since set up a start-up company, Raymei, which plans to launch a larger trial and aims to gain formal approval in three years. “The next clinical trial is pivotal,” he says.
The regeneration of nerve tissue has been one of the great hopes of iPS cells and has been fraught with challenges. Jun Tanga had an office with statues of elephants and navy-blue samurai armour in order to encourage his lab.
He did not set up a company to develop technology for manufacturing the cells and performing the surgery as his wife did. Instead, he has instead transferred that knowledge to Sumitomo Pharma, based in Osaka. “As a scientist, I am kind of satisfied,” he says. He is concentrating on developing cell therapies for stroke.
Some researchers have raised concerns about this fast-track process and related programmes in Japan. Last year, two of the four products that had received conditional approval under this mechanism — one involving thigh-muscle cell transplants for the heart, the other a gene therapy to treat ulcers in narrowed arteries in the limbs — were withdrawn. After a decade on the market, the first was rejected for approval because it did not show clinical benefit. The second was withdrawn after five years because of the data not reproducing what was observed in earlier trials.
Companies can offer the treatments, with costs mostly covered by the national health system. But they must continue to collect data on safety and efficacy to earn full clinical approval.
Although clearly riskier than the usual process, in theory, this system allows potentially life-changing interventions to be provided more quickly to people for whom alternative treatments aren’t available. This is one of the reasons why it is being watched around the world. The other reason is that there is a perception in many countries that conventional regulation is holding back innovation. The first examples of the fast-track process suggest that speed should be held to a high standard.
Early Stage Clinical Trials: The Two-Agent Robot Model that Masayo Takahashi Used to Make her Transplants for a Childhood Neurodegenerative Disease
A white, muscular-looking, two-armed robot is the portable model that Masayo Takahashi used to make her treatments. Powered by machine learning, it checks in on cells’ progress as they are prepared for transplant through a microscope. It can make enough cells in four months to give 800 individual treatments.
The two studies published this week offer hope for people with a disease that is currently only manageable; there is no cure. Such early-phase clinical trials are a crucial part of both the research and the regulatory journey. Subsequent trials are important because they assess whether a therapy can benefit patients.
The early stage clinical trials that reported the results show that interventions were safe and that recipients experienced measurable improvement in symptoms such as tremors and rigid movements.